ANTIBIOTICS RESISTANCE
Some of these mutations make microbes less susceptible to the effects of antimicrobials, a phenomenon known as antimicrobial resistance.
(WHO) defines antimicrobial resistance (AMR) as “resistance of a microorganism to an antimicrobial drug that was originally effective for treatment of infections caused by it.” Resistance occurs when an antimicrobial has lost its ability to effectively control or eliminate a microbial infection against which it was once effective. The microbes are then considered “resistant” and are able to continue to replicate even when the antimicrobial is present.
While many people are aware that bacteria can develop antibiotic resistance, resistance also occurs in viruses, parasites, and fungi. Approximately 700,000 deaths worldwide can be attributed to AMR each year, a figure that is poised to jump to 10 million by 2050 if actions are not taken to combat its spread.
HOW DOES AMR OCCUR?
Some microbes are pre-programmed to be resistant to certain types of antimicrobials. This is known as inherent or intrinsic resistance. For example, Gram-negative bacteria have a cell wall covered by an outer membrane that physically blocks some antibiotics from working. Microbes can also acquire genes that code for resistance, known as acquired resistance, through two ways:-
(1)spontaneous gene mutation during replication (vertical transmission) (2)exchange of genes between microbes (horizontal transmission) Genetic mutations are rare spontaneous changes or errors that happen when microbes replicate. Occasionally, these mutations will confer a change in the microbe that helps it resist the effect of an antimicrobial. These new resistant genes are then passed on to the microbe’s progeny, a process known as vertical transmission.
Microbes can also acquire resistance through horizontal transmission, in which genetic material is exchanged between microbes. For example, when bacteria come in direct contact with each other, small circular pieces of DNA found in the cytoplasm (plasmids) may be transferred through a process known as conjugation. While this is thought to be the main mechanism of horizontal transmission, bacteria may also pick up bits of DNA from the external environment (transformation), or through the transfer of DNA from bacteria-specific viruses known as bacteriophages (transduction). The graphic below illustrates how microbes can become resistant through both vertical and horizontal modes of transmission.
Molecular Mechanisms of Resistance
At a molecular level, microbes have developed several key ways to resist the effects of antimicrobials:
Molecular Mechanisms of Resistance
1.The microbe physically blocks or removes the antimicrobial from the cell.
2.The microbe alters the target site so that it is no longer recognizedicrobe chemically modifies the antimicrobial.
Drivers of AMR:-
unnecessary and inappropriate use of antimicrobials exacerbates the development and spread of AMR.
Drivers of AMR.
Improper use in humans. Globally, more than 50% of medicines are prescribed, dispensed, or sold inappropriately. Overuse and misuse of antimicrobials is a huge global problem resulting from complex and interacting deficiencies across all levels of the health system, including legislation and regulation, supply chain management, quality assurance, prescribing and dispensing practices, and patient behavior.
Improper use in animals. Antimicrobial products are used extensively for agricultural purposes, including the treatment and prevention of illnesses and for increased growth promotion. In fact, animals consume twice the amount of antibiotics that humans do. Most antibiotics used in agriculture are also deemed medically important for use in humans. In the United States, of the 41 antibiotics that are approved for use in food-producing animals, 31 are categorized as medically important for humans.
Accumulation in the environment. Excessive and inappropriate use of antimicrobials in both humans and animals also means that these compounds are accumulating in the environment—for example, through wastewater and runoff. The impact of such accumulation on the emergence of antibiotic resistance should not be understated. Most legislation on water quality does not include provisions to monitor the concentrations of antimicrobial-resistant microbes in sewage or treatment plants.
Selective pressure :-The multiplication of resistant microbes when antimicrobials kill susceptible ones.
The Impact of AMR on Specific Diseases
Tuberculosis, malaria, and hospital-acquired infections (also known as nosocomial infections) The Impact of AMR on Specific Diseases:- Tuberculosis, malaria, and hospital-acquired infections (also known as nosocomial infections), which can be difficult to treat even with effective first-line agents, have become huge burdens on health systems as resistance has increased.
Tuberculosis:
DOTS is the World Health Organization-recommended TB control strategy, which combines five major elements: political commitment, sputum smear microscopy services, uninterrupted drug supplies, recording and reporting systems, and direct observation of treatment.
Multidrug-resistant tuberculosis (MDR TB)
A mutant form of TB that is resistant to at least two of the primary treatment drugs, including isoniazid and rifampicin.
There is currently no content classified with this term.
Extensively drug resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin).
Pneumonia can be caused by multiple types of pathogens, including bacteria, viruses, and fungi. The most common cause of pneumonia in children is Streptococcus pneumoniae (S. pneumoniae).
For many years, pneumonia was cured inexpensively with penicillin. However, resistant strains were identified only four years after penicillin's introduction. Potential complications caused by gonorrhea include the following:
Infertility
Eye (ophthalmic) infections in newborns
Pelvic inflammatory disease
Five-fold increase in HIV transmission
Once easily treatable, gonorrhea is now resistant to several antibiotics, including penicillin, tetracycline, and fluoroquinolones.
Methicillin-resistant Staphylococcus aureus (MRSA) refers to a strain of S. aureus (a common cause of skin, wound, and blood infections) that has acquired genes that can withstand the effects of several types of antibiotics. MRSA began emerging during the 1960s and was primarily seen in hospital-acquired infections. Today, instances of community-acquired MRSA have increased significantly in many countries.
Carbapenem-resistant Enterobacteriaceae (CRE) are a family of bacteria that are difficult to treat because they have high levels of resistance to antibiotics. Klebsiella species and Escherichia coli (E. coli) are examples of Enterobacteriaceae, a normal part of the human gut bacteria, that can become carbapenem-resistant.
*multiple drug-resistant infections (including Pseudomonas aeruginosa, Klebsiella pneumoniae, Morganella morganii, and Enterococcus). His infection tested positive for New Delhi metallo-beta-lactamase-1 (NDM-1), an enzyme which makes bacteria resistant to carbapenems, one of the strongest classes of antibiotics.Artemisinin-based combination therapy (ACT).
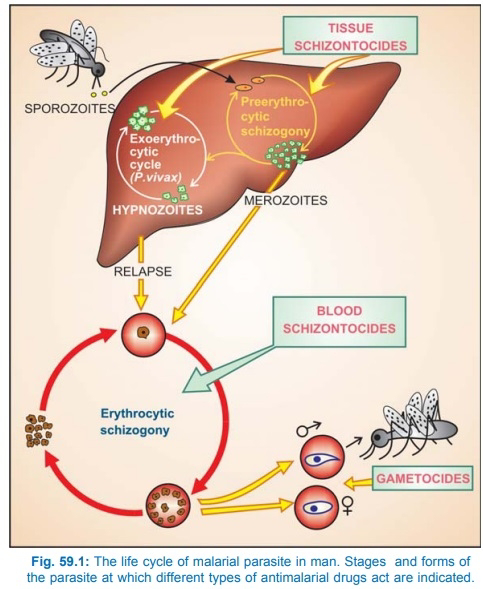
Malaria case management in pregnancy during the second and third trimesters but using quinine during the first trimester.
Effective drugs are needed for Plasmodium falciparum malaria because the disease can be fatal to both the mother and the newborn
Some infections, like candidiasis, are caused by fungi. Candidiasis frequently develops in patients receiving intensive antibacterial therapy and is caused by the yeast Candida, which is the most common cause of fungal infections worldwide.
Antifungal agents exist to treat Candida and other fungal infections. However, some fungi have developed resistance and no longer respond to these medications. Some types of Candida are now resistant to first- and second-line medications, namely fluconazole and echinocandins (anidulafungin, caspofungin, and micafungin).
While rates of fluconazole resistance have remained relatively stable (~7%), echinocandins resistance appears to be increasing (~1% of all Candida cases). For patients who develop Candida infections that are resistant to both fluconazole and echinocandins, there are few remaining treatment options, some of which can be toxic for patients who are already extremely sick.
Necrotizing pneumonia
Necrosisisdeath of body tissue; it occurs when there is not enough blood flowing to the tissue, whether from injury, radiation, or chemicals. Necrotizing pneumonia is a pneumonia characterized by the development of the necrosis within infected lung tissue
Only about half of all malaria cases receive the recommended first-line antimalarial agents. Similarly, only 50% to 70% of pneumonia cases are treated with appropriate antibiotics.
Vancomycin-resistant enterococci
Bacteria that are normally present in human intestines and the female genital tract, and can sometimes cause infection. Vancomycin is a drug used to treat these infections, but some enterococci have become resistant to this drug; they are called vancomycin-resistant enterococci (VRE). Most VRE infections occur in hospitals.
Xpert MTB/RIF
A rapid, fully automated diagnostic molecular test. It simultaneously detects TB and rifampicin drug resistance
Multivalent pneumococcal conjugate vaccine
A preparation of capsular polysaccharide from specific serotypes of Streptococcus pneumoniae that are covalently linked to carrier protein.
Use of multivalent pneumococcal conjugate vaccine in infants and children not only prevents infections, but also significantly reduces drug resistance in Streptococcus pneumoniae.









Comments
Post a Comment